Latest posts
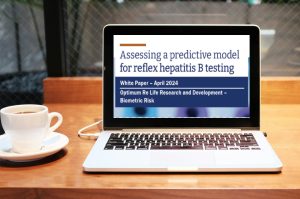
White Paper: Optimum Life Re finds potential 2.5x increased detection of hepatitis B through an improved reflex rule
ExamOne® recently sought to produce a better reflex rule for hepatitis B screening in life insurance using predictive modeling. In a new study, Optimum Life Re evaluates the performance of the ExamOne model in comparison with conventional reflex rules that are solely based on the results of liver function tests.
Drinking and life insurance: Laboratory insights help identify the rising risk of alcohol abuse
A cost-effective test to identify and properly price alcohol risk is the blood alcohol concentration (BAC) assay. Simply adding this to your testing profile provides blood alcohol values and an indication of your applicant’s recent alcohol intake.
LabPiQture provides critical information regarding CKD to insurers
How can insurers quickly and confidently determine if their applicant has kidney disease? In a recent case study, we show how eGFR results highlighted in LabPiQture uncover or disprove chronic kidney disease.
Taking ExamOne to the NEXT LEVEL: employee awards and giving back at annual convention
Join us in appreciating our employees who won awards and those who demonstrated our commitment to our communities by giving back at our recent annual employee convention.
Mapping cholesterol trends for life insurance applicants
Laboratory results from a paramedical exam can help bring awareness of heart health issues to both life insurers and consumers. ExamOne discovers cholesterol trends for life insurance applicants.
3 ways to help “insure your love” in February
Now is the perfect time to encourage your clients to protect their loved ones through proper life insurance planning. See three ways you can help your clients show their love with life insurance.