November is National Diabetes Month. Earlier this year we became the first laboratory in the insurance industry to update our insurance profile to include HbA1c (commonly referred to as A1c) testing for all life insurance applicants. By upgrading to this test, we will help insurers identify more applicants who are either diabetic or who may be in the pre-diabetic stage and not even be aware of it.
This segment of “Ask the Expert” is from our laboratory expert, Betsy Sears, Vice President Laboratory Strategy and Sales. Betsy explains the effects of diabetes on an individual’s body and why we decided to add A1c testing on all applicants.
What occurs physiologically in the body when one has diabetes?
The body breaks down the sugars and starches you eat into a simple sugar called glucose, which it uses for energy. Insulin is a hormone that the body needs to get glucose from the bloodstream into the cells of the body.
In type 1 diabetes, usually diagnosed in children and young adults, the body does not produce insulin.
In type 2 diabetes, your body does not use insulin properly. This is called insulin resistance. At first, your pancreas makes extra insulin to make up for it. But, over time, it isn’t able to keep up and can’t make enough insulin to keep your blood glucose at normal levels.
Why is A1c used as the standard for diabetes diagnosis?
A1c is considered the gold standard for diabetes diagnosis according to the American Diabetes Association. Additionally, screening with A1c alleviates the need for the applicant to fast in order to get accurate blood results. Not having to fast means the applicant has a wider choice of appointment times and the paramedical exam can be completed sooner. (Download our fasting white paper to learn more on how fasting won’t affect the results of an applicant’s paramedical exam.)
Is the A1c test affected by pre-analytic conditions such as heat and time?
No, A1c is stable for the life of the purple top at the lab–28 days. Because A1c testing is part of our routine risk assessment screen now, every specimen is tested upon arrival at the laboratory.
What is an acceptable A1c range?
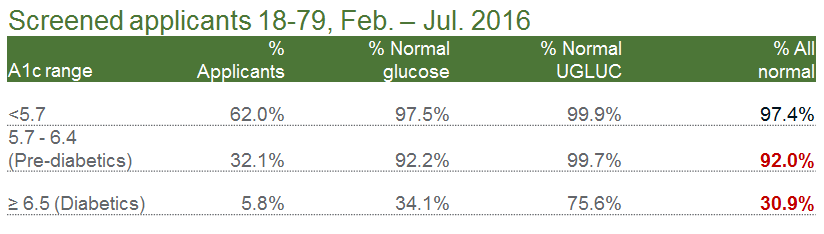
A normal A1c test result is considered to be less than 5.7% of total hemoglobin. The table below demonstrates the percentage of screened applicants (ages 18-79 tested from February 2016 – July 2016) that showed elevated A1c results even in the presence of normal “traditional” reflex markers.
Are there any factors that could affect the interpretation of A1c test results?
Yes. Any condition that shortens erythrocyte survival or decreases mean erythrocyte age (e.g., recovery from acute blood loss or hemolytic anemia) may falsely lower A1c test results. Causes of shortened erythrocyte lifetime include: hemolytic anemia or other hemolytic diseases, homozygous sickle cell trait, pregnancy, recent significant or chronic blood loss. Caution should be used when interpreting the A1c test results from patients with these conditions.
Do you see a high rate of non-disclosure among your applicants with diabetes?
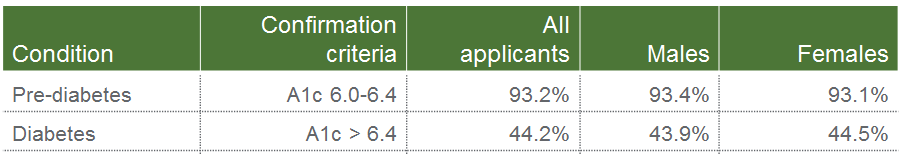
Yes. In a recent study of ExamOne life insurance applicants from 2014 to 2016, an astounding 44% of applicants did not acknowledge they had diabetes. By running an A1c screen, these applicants were identified and underwriters were able to more accurately assess an applicant’s mortality risk based on their laboratory results. Additionally, it should be noted that more than 93% of applicants were found to be pre-diabetic with an A1c screen. There is a chance this population segment didn’t disclose their diabetes condition simply because they were not aware of it existing. The table below highlights more information.












November is National Diabetes Month. Earlier this year we became the first laboratory in the insurance industry to update our insurance profile to include HbA1c (commonly referred to as A1c) testing for all life insurance applicants. By upgrading to this test, we will help insurers identify more applicants who are either diabetic or who may be in the pre-diabetic stage and not even be aware of it.
This segment of “Ask the Expert” is from our laboratory expert, Betsy Sears, Vice President Laboratory Strategy and Sales. Betsy explains the effects of diabetes on an individual’s body and why we decided to add A1c testing on all applicants.
What occurs physiologically in the body when one has diabetes?
The body breaks down the sugars and starches you eat into a simple sugar called glucose, which it uses for energy. Insulin is a hormone that the body needs to get glucose from the bloodstream into the cells of the body.
In type 1 diabetes, usually diagnosed in children and young adults, the body does not produce insulin.
In type 2 diabetes, your body does not use insulin properly. This is called insulin resistance. At first, your pancreas makes extra insulin to make up for it. But, over time, it isn’t able to keep up and can’t make enough insulin to keep your blood glucose at normal levels.
Why is A1c used as the standard for diabetes diagnosis?
A1c is considered the gold standard for diabetes diagnosis according to the American Diabetes Association. Additionally, screening with A1c alleviates the need for the applicant to fast in order to get accurate blood results. Not having to fast means the applicant has a wider choice of appointment times and the paramedical exam can be completed sooner. (Download our fasting white paper to learn more on how fasting won’t affect the results of an applicant’s paramedical exam.)
Is the A1c test affected by pre-analytic conditions such as heat and time?
No, A1c is stable for the life of the purple top at the lab–28 days. Because A1c testing is part of our routine risk assessment screen now, every specimen is tested upon arrival at the laboratory.
What is an acceptable A1c range?
A normal A1c test result is considered to be less than 5.7% of total hemoglobin. The table below demonstrates the percentage of screened applicants (ages 18-79 tested from February 2016 – July 2016) that showed elevated A1c results even in the presence of normal “traditional” reflex markers.
Are there any factors that could affect the interpretation of A1c test results?
Yes. Any condition that shortens erythrocyte survival or decreases mean erythrocyte age (e.g., recovery from acute blood loss or hemolytic anemia) may falsely lower A1c test results. Causes of shortened erythrocyte lifetime include: hemolytic anemia or other hemolytic diseases, homozygous sickle cell trait, pregnancy, recent significant or chronic blood loss. Caution should be used when interpreting the A1c test results from patients with these conditions.
Do you see a high rate of non-disclosure among your applicants with diabetes?
Yes. In a recent study of ExamOne life insurance applicants from 2014 to 2016, an astounding 44% of applicants did not acknowledge they had diabetes. By running an A1c screen, these applicants were identified and underwriters were able to more accurately assess an applicant’s mortality risk based on their laboratory results. Additionally, it should be noted that more than 93% of applicants were found to be pre-diabetic with an A1c screen. There is a chance this population segment didn’t disclose their diabetes condition simply because they were not aware of it existing. The table below highlights more information.